Voice Team Locator
A Voice Team Locator was developed to help teachers easily find voice teams (physicians and speech-language pathologists with specialty training in voice). The directory is organized geographically state-by-state to make it an easy-to-use resource.
Rx and your voice
Could your prescription drug be affecting your voice? Check the alphabetized summaries of the most frequently prescribed medications and their possible effects on vocal health to see if so.
The unwell voice
Vocal problems are common — about 10-20% of all children and 7% of all adults have voice disorders at any given time. (The incidence for teachers alone is higher — about 15%.) The causes of these problems, however, are quite varied. Voice disorders can be caused by disease, injury, over-use or environmental exposure.
Symptoms for most voice disorders are remarkably similar:
- hoarseness;
- difficulty making high pitches;
- voice breaks;
- aching and tiredness in the throat;
- difficulty making soft sounds;
- a feeling of "effortfulness" when using the voice; and
- low volume or complete loss of voice.
The key to correcting most voice disorders is to get medical help if the problem doesn't resolve promptly. Sometimes what you thought was just a hoarse voice due to an ordinary virus or an episode of over-use could be a symptom of something bigger.
Signal of disease: Because teachers are prone to voice problems, it's easy to imagine that fatigue or overuse are always its cause. However, a teacher's problematic voice could be the symptom of another, and possibly, serious illness. When it comes to disease, teachers face the same risks as the general population. Many medical circumstances can impact how the voice sounds. Consider that your larynx is located on the "super highway" of important body parts: your heart, lung, nervous system.
Diseases that show up in the voice (as hoarseness, tremors or other voice changes) include:
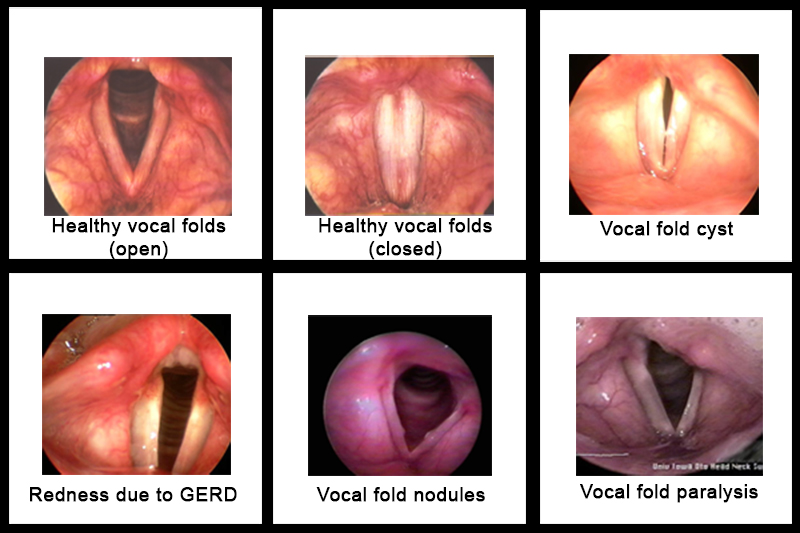
- gastroesophageal reflux disease (GERD);
- larynx cancer;
- endocrine dysfunction, such as hypothyroidism; and
- nervous and musculoskeletal system disorders, such as Parkinson disease.
Unsure? See your doctor.
How the voice gets hurt: Voice trauma doesn't necessarily mean a blow to the neck. More often, vocal disorders due to trauma stem from the lengthy and winding configuration of the laryngeal nerves.
The right and left recurrent laryngeal nerves power most of the vocal fold muscles. They travel from the base of the skull into the neck, down through the upper chest, and back up to the vocal fold muscles in the neck. This long path makes the laryngeal nerve vulnerable to a serious traumatic injury: vocal fold paralysis. If there is nerve injury, your physician must understand the circumstances of the injury and any resulting difficulties. A thorough medical examination, usually along with imaging studies, is essential.
Can your voice hold up? Face it: our bodies are uniquely composed with differing strengths, weaknesses, tolerances and fragilities. Teaching places a high demand on even the most resilient vocal system. Besides over-use (in politically correct terms, a "vocal overdoer"), damage can arise from excessive throat clearing, coughing, inhaling irritants (a problem especially for art, industrial education or chemistry teachers), smoking, screaming, yelling, or speaking too loudly or at an abnormally high or low pitch. If a teacher's larynx is inherently fragile, s/he needs to be a diligent manager of vocal health to meet the intensity of teaching. You are your vocal system's chief executive officer. With the right information and motivation, about 75% of teachers' voice problems can be prevented or self-managed. Don't undermine your important role in vocal health.
Everyday illnesses
Colds and sore throats: It is the rare, lucky teacher who avoids catching at least one nasty cold or virus per year. The close proximity and questionable hygiene of young people besieged with viruses place the teacher at great risk of contamination. Caused by viruses, colds easily travel in a closed atmosphere such as a classroom. They typically last 4-6 days and can cause a sore throat, hoarseness, laryngitis or respiratory infection. The best way to prevent a cold is to build a healthy body: exercise, eat right and rest well. If you catch a cold, take it easy. Relax, eat lightly, and blow your nose gently to prevent further sinus or middle ear problems.
You may feel it's impossible to skip a day, but bed rest is the best medicine for a cold. Let your body heal itself, and don't spread the infection to your co-workers or students.
Allergies and other damp conditions: For teachers with allergies, management is key — and protecting your voice is a high priority. An allergy is the hyper-sensitive response to something in your environment. The allergen usually produces swelling of the mucous membranes in the nose and mouth, which may interfere with vocalization. Once you know the offender, you can try to avoid it. Barring that, medications can help. If allergies are more than a mild annoyance, you would benefit by working one-on-one with a physician with specialized training in these conditions (an allergist).
Beware of the dual-edge of antihistamines: While antihistamines dry up mucous secretions (and make you feel better), they dehydrate voice tissues. If you use them, sip water throughout the day.
What to expect at a voice center
If you need a voice check-up, your visit likely will be in three parts: a medical history; examination of the vocal folds; and voice assessment and possible treatment. At your check-up, it is important to give detailed information on overall health status, medications, allergies, voice use, eating habits, sleep patterns and any concerns you may have. Even subtle clues could be at the root of a voice disorder.
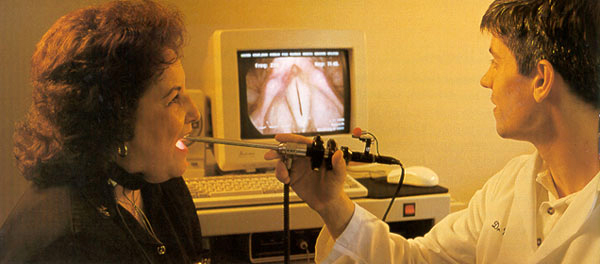
Your vocal folds will likely be examined via videostroboscopy, a tool used to view the vocal folds in motion. This amazing instrument allows your otolaryngologist (ENT doctor) to get a good look at your larynx, and especially, your vocal folds. Although it's a bit awkward, the patient can make a few sounds (usually, an "ee") so that the doctor and speech-language pathologist can see the vocal folds in motion. A permanent, digital record of the exam is usually stored as part of your medical record.
What's voice therapy? Teaching people how to correctly use their voices is nothing new. Vocal pedagogy — for actors and singers — originated in the middle ages. Teachers who knew nothing about vocal anatomy advised students based upon what they saw and heard. The result: an emphasis on articulation, pitch, projection and proper breathing techniques. Modern speech-language pathologists can use those same elements — along with ever-increasing scientific and medical knowledge of the voice -- to provide care. Ideally, the speech-language pathologist focuses on habilitation (optimal usage of the voice under less than ideal circumstances) as well as rehabilitation (repair).
Phonosurgery: Surgery performed to improve the voice is called phonosurgery. Its success is highly correlated with the experience of the surgeon. Physicians specializing in ear-nose-throat conditions (otolaryngologists), AND sub-specializing in voice surgeries are called laryngologists.
Surgery is appropriate for only some voice patients, usually if:
- visible lesions are diagnosed;
- the lesions don't respond to therapy;
- the lesions don't respond to therapy;
- the post-therapy impairment is unacceptable to the patient;
- the client and voice team believe the surgery can help.
Phonosurgeries are often: laryngeal microsurgery (removal of small lesions); or medialization surgery (moving and/or injecting material to improve closure of the paired vocal folds).
Acid rain from the stomach
Reaching for antacids a lot lately? Your stomach may not be the only thing that needs to be checked out. Gastroesophageal reflux disease (GERD) can significantly impact your voice. GERD is increasingly named as a culprit in voice disorders. One study found GERD to be a problem in more than three-quarters (78%) of patients with hoarseness and half of all patients with voice complaints. The problem arises when stomach acids travel back up through the esophagus and then irritate the tissue in the back of the throat and larynx. GERD also can indirectly cause voice problems: GERD sufferers sometimes cough or clear the throat frequently, which may harm tissues of the larynx. Others with GERD tend to use excess muscle tension when they speak (in response to the altered feeling in the larynx).
What are GERD's symptoms? Many people associate GERD with heartburn. In reality, however, only about half of all GERD sufferers have heartburn symptoms.
So, what are GERD's symptoms?
- voice hoarseness;
- sour breath (especially upon awakening);
- frequent throat clearing;
- excessive phlegm or saliva, especially in the back of the throat;
- difficulty swallowing food, liquids or pills, and/or a feeling of a lump in the throat;
- coughing after eating or lying down;
- breathing difficulties (such as asthma-like wheezing) or choking episodes;
- dry cough;
- indigestion.
Gain control of GERD: There are three basic approaches to tackling GERD: diet and lifestyle changes; medication; or surgery.
Self-management tips:
- Don't eat or drink anything but water within three hours of bedtime;
- Don't overeat;
- Don't recline after meals;
- Eat a low-fat diet;
- Avoid fried foods, coffee, tea, chocolate, mints and soda;
- Elevate the head of your bed 4-6 inches or sleep o
- on a wedge-shaped pillow;
- Don't wear tight-fitting clothes or belts;
- Stop smoking
Diseases affecting the voice
Cancer: Symptoms include voice change, chronic sore throat, swallowing difficulty or restricted breathing. Treatment depends upon size and location of the tumor, whether it has metastasized, and patient age and health.
Recurrent Respiratory Papillomatosis: This uncurable virus provokes wart-like growths in the vocal tract. Untreated, the lesions can increase in size and bulk until function is severely impaired. Standard treatment is periodic laser vaporization.
Endocrine Dysfunction: A hoarse voice and reduction of pitch range may signal hypothyroidism. Blood samples determine hormonal imbalances. Treatment usually includes medication.
Nerve or muscle system diseases include vocal tremor; vocal fold paralysis; and spasmodic dysphonia (uncontrollable squeezing of laryngeal muscles). SD is treated with periodic injections of botulinum toxin into the problem muscles.
Trauma's impact on the larynx
Vocal fold scarring: Poorly performed surgery is the most common source of vocal fold scarring. This can result in chronic hoarseness, double pitch in the upper singing pitch range and limitations of vocal capabilities.
Although voice building and conditioning can reversed this condition to some degree, they will not restore normal mucosal vibration.
Bodily injuries: Initial diagnosis of most bodily injuries occurs in a hospital emergency room. Voice-producing structures may be crushed or otherwise damaged. Injuries involving the larynx will most likely be evaluated in the outpatient office of an otolaryngologist.
The goal of all traumatic injuries is to preserve functions as near to normal as possible.
Vocal overload
Laryngitis: This is inflammation or swelling of the vocal folds caused by excessive use of the voice, infections, or irritants. The vocal folds — in a swollen state — cannot vibrate normally, sounding raspy, breathy and hoarse.
Nodules: Small callous-like growths on the vocal cords result when the vocal folds are forced together harshly over a long period of time, resulting in breathy, raspy and low-pitched voice. Vocal rest and voice therapy are most often prescribed.
Polyps: Similar to vocal nodules, but nodules are more like callouses and polyps like blisters. Voices are low-pitched, hoarse and breathy.
Contact ulcers: Less common, these result from reflux disease or forceful vocal fold closure. Ulcers may result from frequent harsh throat clearing.
Cysts: These resemble tiny "skin tags" in the vocal fold, causing hoarseness and loss of high pitch ranges.
Long-term irritants
Reinke's edema: Also known as smoker's polyps, these growths result in lower vocal pitch range and thickened voice quality.
Women with smoker's polyps may find themselves being called "Sir" on the telephone.
On occasion these grow large enough to restrict the airway.
While smoking cessation helps stop polyp growth, normal vocal capabilities may never be attained.